Risk information about medicines is too important to end up at the bottom of a pile of mail at healthcare providers. The MEB therefore participated in a pilot project in 2017 to send important new risk information by email. This pilot project is a collaboration between the Health and Youth Care Inspectorate (IGJ) (formerly IGZ), the Dutch Institute for Rational Use of Medicine (IVM) and the Pharmacovigilance Centre Lareb.
“This pilot project is in line with the MEB's activities: we are vigilant, we wish to share the latest scientific knowledge and, in doing this, we remain in close contact with healthcare providers.”
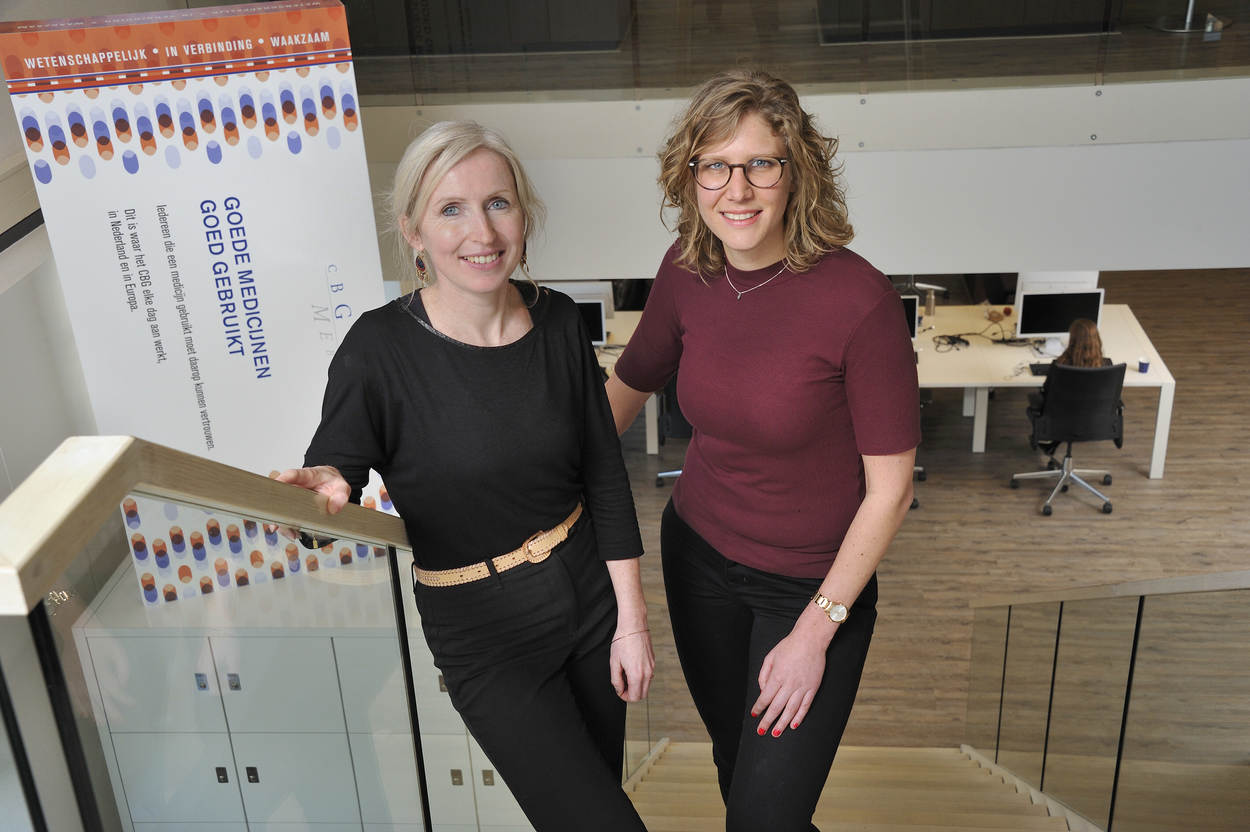
“This pilot project is in line with the MEB's activities: we are vigilant, we wish to share the latest scientific knowledge and, in doing this, we remain in close contact with healthcare providers,” according Nanneke Hendricks, programme manager of the Better Use programme. She was involved in the pilot project as a MEB representative together with Inge Zomerdijk (assessor pharmacovigilance and now project leader of the Better Use programme).
Healthcare providers receive a many different notifications every year with important new information about medicines. Pharmacovigilance is one of the MEB's statutory duties, and consequently, the MEB is obliged to inform healthcare providers about important risk information regarding medicines. In some cases, it is important that healthcare providers are informed immediately. At present, healthcare providers receive this important risk information from the responsible pharmaceutical company, i.e. the ‘Direct Healthcare Professional Communication’ (DHPC) by post. In addition to this, the MEB publishes a news release on its website with a digital version of the letter and also publishes and distributes a digital newsletter.
It sometimes occurs that patients already know via social media about certain risk information that the healthcare provider has not received yet. Sending the DHPC via a digital channel like email could contribute to informing healthcare providers about important new risk information in a faster and more efficient manner. We tested this in 2017 via the pilot project ‘Important new medicine information’.
Alert via e-mail
New important risk information about medicines from the Dutch Health and Youth Care Inspectorate (IGJ), the MEB and Lareb was sent by email, i.e. the ‘Alert’, to the participants in the pilot project. Around 100 participants including pharmacists, doctors and medical specialists participated in this pilot project. For the MEB, this meant that for every DHPC an alert was also sent to the pilot project participants within the group of healthcare professionals who already received the paper version of the DHPC. In addition to the alerts, the whole group of participants received a monthly newsletter via email with an overview of the alerts that had been sent. The IVM assumed responsibility for the organisation of the pilot project and was responsible for sending out the alerts. The respective organisations remained responsible for the contents of the alerts. The MEB provided a short uniform text for the alert for each DHPC with a link to the DHPC, which was then processed and sent by the IVM.
“The pilot project is part of the MEB programme ‘Better Use’. We also try to make information available for healthcare providers better and faster. I think it is a good thing that the MEB participates in this pilot project and that we critically examine how the project is set up and executed.
In this manner, we ensure that the information is provided to healthcare providers via one channel, instead of healthcare providers having to monitor the individual websites of the IGJ, Lareb and MEB,” Hendricks explains. Inge Zomerdijk adds: “It is actually a small-scale pilot study that is being carried out by another party. Although, we are closely involved and we provide our input on the set up and evaluation of the pilot project.”
Hendricks: “And that is logical. If you look at the number of alerts, I see that about 80% of the alerts that have been sent out are from the MEB.”
Jonneke Verdijk, pharmacist at Radboudumc, received the monthly newsletter and the alerts
“We participated in the pilot project because we knew that the timely receipt and (uniform) handling of alerts and newsletters is potentially risky within a big organisation like Radboudumc. There is the risks that alerts are not received timely or correctly due to the changing working locations of pharmacists, and in the event of recalls, the required actions take a lot of time. In addition, as a pharmacy, we wish to inform healthcare providers. Our experience with this pilot project has been positive. We often received the alerts earlier than other (digital) messages. We received the alerts in a general email box. We make agreements internally about the registration and analysis of these messages. With this way of working, we are better able to ensure that important news items are processed in the organisation.”
Positive
It is clear from this pilot project that the information received via email is appreciated by the target group. Zomerdijk: “The recipients are very positive: it is fast, they can easily store the information or forward it to colleagues or nurses.” At present, the group of 111 participants is too small to draw definitive conclusions.”
The risk information is not intended directly for patients in view of the medical jargon used in this information.
In 2017 we started a risk communication pilot scheme. We set up an extra communication channel for doctors and pharmacists to get important information to the healthcare provider quickly so they can act accordingly and ensure patients are well informed.
The pilot scheme was a success and we'd like to continue it in 2018. All talks we had with doctors and pharmacists revealed that they like to receive new important information about medicines swiftly so they can act accordingly and also inform patients quickly and correctly.
Some want to be informed via email, others via the prescription system or professional associations. But there are also still doctors and pharmacists who like to be informed by letter. So we use all the various ways of reaching the healthcare provider.
And I hope that we can utilise what we learn from the pilot scheme to create a suitable channel via which the information quickly reaches those people who need to know it.
Close cooperation
The cooperation between the parties involved has been intensified and/or further expanded as a result of the pilot project. “We have also learned something from each other. Before the alert, it was challenging for the MEB to describe an indication in three words. The IVM came up with the suggestion to use the term ‘indication area’. I thought this was good solution,” Zomerdijk remarks.
Irene Smeeman, locum GP, received the month newsletter
“I consider it important to remain informed about important medicine information. We GPs receive the information from pharmacies or the FTO later. For this type of important information, you have to make optimal use of the digital possibilities. The newsletter is an excellent way to be informed quickly about important medicine information: It is a well-structured document with a short description of the new information and you can easily find the background information. An ideal way to stay informed without an overkill of specialist information that is not relevant for me. The frequency was also good. As far as I am concerned this is an initiative that may continue to exist. It is good that the institutions that are involved in monitoring the functioning and the adverse effects of medicines issue one clear report together.
Discussion: the sender
The contents of the DHPC are discussed with the IGJ and the MEB; however, the marketing authorisation holder is the official sender of this letter. The pilot project shows that the recipients place more trust in information that comes from the government. Hendricks: “That is why we are also considering the official sender of the DHPC; this is another issue that runs parallel to the pilot project. Pharmaceutical companies have already come up with various suggestions for this. It is also in the pharmaceutical companies’ interest that the information is well received.” When this pilot project has been completed and the procedure for the digital sending of the DHPC has been established, these two projects will be combined.
Follow-up pilot project
The project group aims to gain more experience with a larger group of healthcare providers in a follow-up pilot project in 2018. There are also a number of points for improvement; such as a fast and easy way for the recipients to provide feedback on the alerts and newsletters that have been sent. We are also looking at other channels than email for sending information and what would be a suitable method for the collection and management of an address data base. The follow-up pilot project will be held from March 2018 to the end of August.
The final objective is to distribute risk information quickly in an as efficient and effective manner possible. In addition, the aim is also to ensure an efficient organisation of the sending of risk information by MEB, IGJ and Lareb.
About the pilot project ‘Important medicine information’
In the pilot project, IVM sent an alert by email with a reference to the news release of the IGJ, Lareb or the MEB. 111 healthcare providers participated in the pilot. They received in total 13 alerts and 5 newsletters in the period between 15 June and 15 November 2017. The participants could also find the alerts and newsletters on a website.
In the evaluation, 88% of the 64 respondents stated that the alerts and newsletters that they received had an added value. Many participants regarded the speed as a particular advantage. A number of participants also stated that they would not have received some of the relevant information if they had not participated in the pilot project. 81% of the respondents considers the government to be a reliable sender.